Functions of the kidney
introduction
The kidneys are bean-shaped, paired organs that are in a Variety of functions of the human organism are involved. The most well-known function of the organ is that Urine production. The kidney mainly serves the Regulation of the electrolyte and water balance, but at the same time it also takes on essential functions within the Acid-base balance and the Elimination of toxins. The kidney also plays an important role in the Regulation of blood plasma volume and thus the Blood pressure. Also, hormones like Calcitriol (Calcium balance) or Erythropoietin (Blood cell synthesis) in the kidney synthesized.
Read on under: Function of the kidney
general tasks
The kidney primarily serves the Electrolyte regulation: Various ions such as sodium (Na +), chloride (Cl-), calcium (Ca2 +) and magnesium (Mg2 +) are either excreted / secreted or retained / absorbed. Thus, the kidney ensures that Ions that are important for the body, sufficiently made available will respectively Eliminates surpluses become. Besides, the kidney is for that Elimination of drugs, toxins and metabolic wastes, such as ammonia or uric acid are responsible.
With the excretion or resorption of ions (especially of sodium) is also at the same time excreted water or absorbed. So the volume of the extracellular space and the Affects blood volume become and thus indirectly Influence on the Blood pressure will be taken. Because of this, you can Medication, those who Increase urine production, such as loop diuretics, thiazides or aldosterone receptor antagonists Therapy of high blood pressure (hypertension) can be used.
Read on under: high blood pressure and Medication for hypertension
The acid-base balance of the body is regulated by the elimination of protons (H +) and hydrogen carbonate (HCO3-). This mechanism plays an important role in compensating for acid-base imbalances that can occur, for example, in the context of respiratory acidosis (acidification of the blood caused by breathing). Such acidosis can be triggered, for example, in the context of a stressful situation by increased breathing.
By influencing the phosphate and calcium levels, the kidneys control bone mineralization, i.e. the incorporation of calcium and phosphate into the bones. The hormone calcitriol is also produced in the kidneys and also plays a central role in building bones. In addition to calcitriol, other hormones such as erythropoietin are also synthesized in the kidney. Erythropoietin affects the production of red blood cells.
Kinins, urodilatin, prostaglandins, and renin are also made in the kidney. Kinins are important for regulating the size and permeability of the buttocks in the context of inflammatory processes and for sensitizing pain receptors.
Urodilatin is used to increase blood flow to the kidneys, urine production and the cardiac output.
The hormone renin enables the conversion of angiotensinogen into angiotensin and is thus involved in the regulation of blood pressure.
Prostaglandins have important functions in the development of pain, inflammation, fever and as mediators.
Find out more about the synthesis products of the kidney at: Calcitriol, Erythropoietin and Prostaglandins
Task of the renal cortex
The kidney cortex is located between the kidney capsule and the kidney medulla. The kidney cortex is about 10 mm thick. The blood vessels are located in the renal cortex (Glomeruli), those who first station of urine production represent. The glomeruli consist of a supplying vessel (Vas afferens) and a draining vessel.
Substances that are in the blood (electrolytes, medication, etc.) can be found here from the vessels emerge and between the membranes of the podocytes (star-shaped cells around the capillary) up into the capsule room reach. The filtered plasma liquid (about 150l / day) is called Ultrafiltrate.
The ultrafiltrate first flows through the first section of the proximal tubule (Pars convoluta) and is there in his Composition modulates. You can use different transporters and channels Electrolytes such as sodium, chloride, bicarbonate, potassium and calcium, among others taken from the ultrafiltrate become. Approximately two thirds of the filtered table salt and over 90% of the bicarbonate will be in this section again back into the blood guided.
In the further course will be Proteins, peptides and amino acids reabsorbed. Also be Glucose, galactose and more sugar in the first section obtained from the filtrate.
The pars convoluta of the distal tubule is also located in the cortex, in which the electrolyte concentrations in the urine are finely adjusted.
Functions of the renal medulla
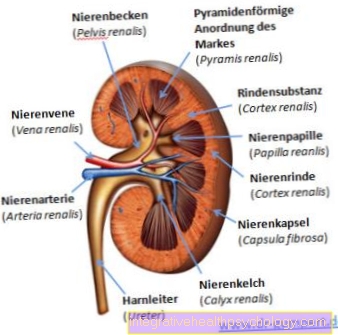
The renal medulla is located between the renal cortex and the renal pelvis. The kidney medulla consists of about ten to twelve tissue pyramids, which are also known as kidney pyramids. These tissue pyramids point outwards with their broad surface, while the tips protrude into the kidney calyx. The kidney pyramids are located in the renal cortex as medullary rays (Radii medullares) continued.
Several collecting tubes run in each of the kidney pyramids. The urine composition is finely regulated in the collecting pipes and water is also reabsorbed. The urinary pores from which the secondary urine drips into the calyx are located at the tip of the kidney pyramids.
In the medullary area there are also the entry and exit points of the blood vessels, which are essential for the transport of electrolytes and substances in and out of the kidney.
Functions of the calyxes
The Calyxes lie inside the kidneys and serve the Urinary diversion. Approximately 10 small calyxes are counted per kidney (Calices renalis minores). Several calices renalis minores form the two large calyxes (Calices renalis majores). The great calyxes form the renal pelvis. There are also two types of kidney calyx: the ampullary and the dendritic calyx. The dendritic calyxes are branched and long, most closely resemble tree roots in their appearance, while the ampullary calyxes are rather short and in comparison wider. They also flow directly into the renal pelvis.
For more detailed information on anatomy, read: Kidney anatomy
The calyxes take up the urine of the collecting tubes and direct this into the renal pelvis further. The Modifications of the filtratesuch as pH changes, absorption and secretion of electrolytes, pollutants and drugs are in the previous tubular systems completed been what the Secondary urine results. At the end of the collecting ducts are the renal papillae from which the secondary urine is slowly and continuously "drips" through pores into the renal pelvis.
The function of the kidney calyx can depend on Kidney stones (Nephrolithiasis) are disturbed, as in this disease the The drainage of the urine is mechanically disturbed is. If the urine cannot flow out, it first collects in the renal pelvis, then in the calyxes and can lead to an enlargement of the kidney calyxes.
Functions of the renal pelvis
The renal pelvis is a Cavity inside the kidneys of the kidney calyx collects dripping secondary urine. This section will no further modification of the urine composition carried out. The renal pelvis is used exclusively for the transmission of urine into the ureter (Ureter), which direct the urine to the bladder.
In the renal pelvis are also Pacemaker cells localized which the Urinary peristalsis regulate the movement of urine through the urethra. In the wall of the renal pelvis there are smooth muscle cells that can contract and facilitate the outflow of urine. At a Urinary diversion disorder (Ureteral stones, pinching of the ureters) the urine can become build up to the renal pelvis and lead to a (painful) enlargement of the renal pelvis. As a result of urinary stones or the resulting urine congestion, inflammation of the renal pelvis (Pyelonephritis) train.
Read on under: Pelvic inflammation and Kidney stones
Urine production

The main task of the kidney is to produce urine. The blood enters the kidneys via the renal artery and enters the glomeruli via the afferent vas. There, electrolytes, amino acids, drugs, toxins, proteins, sugars and much more are filtered out. This ultrafiltrate first flows through the tubular system, in which the substances that are important for the organism are recovered. These are electrolytes (sodium, potassium, calcium, etc.), but also sugars, proteins and amino acids. Harmful substances are left behind in the primary urine or, in some cases, are also actively secreted into the primary urine. This ensures that no important substances are lost and that harmful substances (toxins, metabolic end products, etc.) are excreted.
After the primary urine has been adjusted in terms of its constituents, it is called secondary urine, which flows through the collecting tube through the kidney pyramids to the urinary pores. The secondary urine then "drips" into the kidney calyx and flows off towards the renal pelvis.
Several calyxes open into the renal pelvis. The urine collects in the renal pelvis and is transported from there via the ureters into the bladder. In this context, the pacemaker cells of the renal pelvis serve to regulate the propulsive ureter transport.
Control of urine production
The urine production is controlled mainly by two different hormones: adiuretin and aldosterone.
Adiuretine, also called antidiuretic hormone, is produced in the hypothalamus and enters the bloodstream via the posterior lobe of the pituitary gland.
Adiuretin binds V2 receptors in the distal tubule and in Manifold and increases the incorporation of aquaporin 2 (AQP2) into the membrane. This is Water channelsso that increased water is extracted from the urine and into the bloodstream can get. From this follows one Increase in blood volume and Concentration of the urine.
over V1Receptors on vascular smooth muscle cells are caused by adiuretin to contract. Through the Contraction of the vascular muscle cells and the larger blood volume has adiuretin one antihypertensive effect.
Aldosterone belongs to the renin-angiotensin-aldosterone system (RAAS for short) and is produced in the adrenal cortex. Aldosterone works by stimulating a receptor inside the cells of the distal tubule. Aldosterone does one Increase in the expression of various proteins: Luminal sodium and potassium channels (direction "urinary vessel") and sodium / potassium pumps directed towards the blood vessel. These proteins cause more sodium to be withdrawn from the urine. This creates a gradient that leads to passive recovery of water leads. Potassium, on the other hand, is excreted more.
The basal secretion of aldosterone fluctuates over the course of the day. It can also be regulated by several factors. At a low blood volume (Hypovolemia), one Sodium deficiency (Hyponatremia), one Excess potassium (Hyperkalemia) or when kidney blood flow decreases, aldosterone becomes increased in the bloodstream submitted.
As a result, aldosterone and adiuretin result in less water in the urine; consequently sinks the Urine volume, whereas the Concentration increases. In contrast the blood volume increases and thus secondary to the Blood pressure. In addition, aldosterone and adiuretion influence drinking behavior by promoting a feeling of thirst and thus also leading to increased fluid intake.
Find out more at: Mineral corticoids and Adiuretine
Task in the electrolyte and mineral balance
The kidney serves the Maintaining balance in the mineral salt or electrolyte balance. Electrolytes play a central role in many cell processes, so their concentrations must be strictly regulated. The kidneys have different mechanisms to ensure an optimal balance.
The kidney tends to do the Electrolytes which are in Primary urine are by resorption to win back. The electrolytes are absorbed from the filtrate through various transport systems and channels and can get back into the blood system. So preserved the kidney the organism against unnecessary electrolyte loss.
If the concentration of an electrolyte is too high, for example, the kidneys can increase the excretion of this electrolyte by selectively reducing the absorption of this ion. If the kidney function is disturbed, the electrolyte concentration in the blood plasma can fall outside the normal value, i.e. it can either be increased or decreased. Some drugs, such as diuretics, can block the kidney's transport systems and therefore also lead to electrolyte disorders.
Find out more about the relevant electrolytes: sodium, potassium, Calcium and chloride





















.jpg)
