Therapy ankylosing spondylitis
Note
This topic is the continuation of our topic:
- ankylosing spondylitis
Synonyms in a broader sense
Ankylosing spondylitis (AS), ankylosing spondylitis, spondylarthropathy
Rheumatism, rheumatoid arthritis, psoriatic arthritis, methotrexate
English: Ankylosing spondylitis
Initiation of therapy
The therapy is based on the inflammatory activity and the stage of Bechterew's disease. Furthermore, the doctor must of course take the patient's individual response and comorbidities into account.
As a measure of the disease activity, the BASDAI (B.ath A.nkylosing S.pondylitis D.isease A.ctivity I.ndex). It is a patient questionnaire that was developed in 1994 by a group from Bath, England. The question is e.g. according to the duration and severity of the Morning stiffness, Pain and fatigue.
Therapy goals are the slowing down of the inflammatory process, counteracting the stiffening tendency of the Spine, Pain relief and, if possible, the preservation of function and strength of the joints.
physical therapy
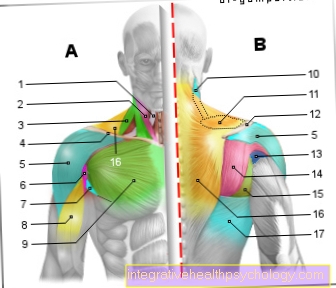
Through physiotherapy (physiotherapy) the mobility of the joints is improved or maintained, shortened muscle groups are stretched and weakened muscles are strengthened. Furthermore, coordination is trained, evasive movements are learned and pain is reduced.
Recommended sports are:
- swim
- To go biking
- Cross-country skiing
- Forest run and
- Volleyball.
Strong vibrations, one-sided loads, sports with a high risk of injury and sports with increased kyphosis (hump formation) should be avoided Spine (correct handlebar setting when cycling!).
General information on physiotherapy can be found under our topic:
- physical therapy
- specific information is available from Medon.de - Physiotherapy for Bechterew's disease
Physical therapy
Physical therapy measures are e.g. Heat / cold applications, medical baths, massage, Electrotherapy, Ultrasound, etc. They are primarily used for pain relief and Muscle relaxation.
Medical therapy
Nonsteroidal anti-inflammatory drugs (NSAIDs) and COX 2 inhibitors (such as Arcoxia® 90mg) are the basis of the drug therapy of Mb. Bechterew. They lead to pain relief in 60-80% of patients and probably also have a positive effect on stiffening.
Long-term disease modifying antirheumatic drugs (DMARDs), which are essential for patients with rheumatoid arthritis, have almost no effect on the inflammatory changes in the spine in ankylosing spondylitis. The best-studied drug from this group for Bechterew's disease is sulfasalazine (e.g. Pleon®). It has been found that patients with low disease activity and predominant involvement of the spine usually do not benefit from treatment with sulfasalazine, whereas patients with predominantly peripheral joint inflammation and patients in a highly active early stage of spinal involvement may benefit from treatment.
Occasionally, ankylosing spondylitis patients are also treated with methotrexate. The effectiveness of methotrexate is judged very contradictory. The effect of methothrexate seems to be essentially limited to the peripheral joints, i.e. knee joint, hip joint, shoulder joint, etc.
For more information on methothrexate, see our topic: Methotrexate
In contrast to rheumatoid arthritis, systemic S.teroids (cortisone) hardly with ankylosing spondylitis. However, in the event of acute involvement of one or a few joints, the doctor can perform intra-articular injections (injection into the joint) of local anesthetics (= local anesthetics) and steroids (cortisone).
This often leads to rapid pain relief and maintenance of the function of the joint. If there is insufficient improvement after steroid injection, a radiosynoviorthesis (RSO = obliteration of the inflamed joint mucosa with radionuclides, e.g. yttrium 90, rhenium 186 or erbium 169) or chemosynoviorthesis (CSO = obliteration of the inflamed joint mucosa with so-called sclerosing drugs) or osmric acid medication can be performed become. Tendon attachments can be infiltrated locally with a local anesthetic and, if necessary, a water-soluble steroid (cortisone).
You can find more information about chemosynoviorthesis under our topic: Chemosynoviorthesis.
In recent years it has been shown that therapy with TNF-alpha inhibitors (e.g. Humira®, Remicade®, Enbrel®) shows good effectiveness in active ankylosing spondylitis. According to the recommendations of the ASAS (Assessments in Ankylosing Spondylitis) group, an international group of researchers, mostly rheumatologists, therapy with TNF-alpha inhibitors should be started if the diagnosis of ankylosing spondylitis (confirmed by a rheumatologist) is certain, A BASDAI> 4 was present for at least 4 weeks and if at least two different nonsteroidal anti-inflammatory drugs for three months, an intraarticularly injected steroid or sulfasalazine do not show the desired effect in patients with predominantly peripheral joint inflammation.
Contraindications for the use of TNF-alpha inhibitors such as Tuberculosis or other severe infections and moderate to severe heart failure must be ruled out by the doctor in advance.
You can find more information on the subject of heart failure under our topic: Heart Failure
More recent studies exist on the effectiveness of thalidomide and pamidronate in the drug treatment of ankylosing spondylitis. For a well-founded assessment, however, further study results must first be awaited.
Operative therapy
In operative therapy measures, a distinction must be made between preventive, reconstructive and palliative interventions. The aim of all surgical therapy measures is to reduce pain, maintain or restore joint functions and maintain a horizontal line of sight.
The choice of procedure depends on the degree of joint destruction or degree of stiffening. Most interventions in the orthopedic rheumatology can be carried out in a planned manner. In principle, however, not every possible intervention is profitable for the patient. The surgical method, follow-up treatment, chances of success and options for retreating should definitely be discussed with the surgeon in advance.
In the area of the peripheral joints with largely intact cartilage conditions, there is an indication for surgical therapy if swellings persist for more than 6 weeks despite optimized drug therapy that has been adapted to the current condition. The inflamed synovial membrane is then removed arthroscopically or openly, as radically as possible, depending on the joint. Synovectomy).
After an arthroscopic synovectomy, it is useful to prevent re-inflammation of the joint, 6-8 weeks after the operation RSO (Radiosynoviorthesis) or CSO (chemosynoviorthesis) to connect.
In younger patients there is limited cartilage damage, but severe axial deviations Joint surface correcting interventions (Adjustment osteotomies) are used. The aim is to achieve an even load on the joint parts again or, in the case of limited cartilage damage, to remove it from the main load zone. For this purpose, the bone is severed and stabilized in the corrected position with screws / plates / wires. These interventions are usually combined with a synovectomy.
Advanced stages with the corresponding joint destruction usually require joint resection, joint replacement or joint stiffening interventions.
At a joint resection surgery The destroyed joint parts are removed, the joint surface is reshaped and replaced with an interposal made from the body's own tissue (e.g. capsular tissue, fatty tissue, muscle fascia). However, such procedures are not possible on the large joints that bear the body weight (knees, hips), as they would not withstand the load. Such interventions are usually carried out on the forefoot or Elbow.
Joint replacement surgery are now possible on almost all joints. The destroyed joint parts are removed and replaced by an artificial joint (endoprosthesis, Hip prosthesis, Knee prosthesis) replaced. Depending on the age, general condition and mobility of the patient and the quality of the bone, cementless or cemented endoprostheses can be used.
In the case of joint instability, a coupled system may have to be used or the ligamentous apparatus stabilized. With the joint replacement surgery, a very good pain reduction is achieved, and after appropriate physiotherapy exercise treatment, good mobility and rapid resilience are achieved. The disadvantage is the limited durability of the endoprostheses.
Joint stiffening interventions create a stable and difficult situation. The destroyed joint surfaces are removed, the joint partners are placed on top of one another in a functionally favorable position and fixed with plates / screws / nails or wires until ossification / stiffening has occurred. They are usually performed when a joint replacement is not possible or is no longer possible, often primarily on the toes, fingers, hand and ankle joints and on the spine.
In the field of Spine there is an urgent indication for surgical therapy in the case of neurological disorders (sensorimotor deficits in arms and legs, tetra- or paraspasticity, unsteady gait, increased muscle reflexes). Operations in the case of bony instabilities are relatively urgent if the decompensation of the statics affects the patient's field of vision and endangers him in everyday life. Further indications for a straightening spondylodesis (stiffening operation on the spine with axis correction) are severe pain or if a horizontal line of sight can only be achieved by bending Knee joint to be reached.
With all surgical measures there are general and special risks which the surgeon informs the patient about before the planned interventions. Some, such as the risk of a Wound infection or Wound healing disorder, are increased in patients with ankylosing spondylitis from the disease itself or from drug treatment. Therefore, before a planned surgical procedure, you should definitely talk to the doctor about a necessary dose reduction or discontinuation of the medication.
rehabilitation
For the success of the above rheumatic orthopedic surgery is one intensive follow-up treatment essential.
The follow-up treatment regimen is usually determined by the surgeon. This includes, on the one hand, regular wound checks and dressing changes, and, on the other hand, depending on the procedure, special follow-up treatment in the form of physiotherapy, possibly with the use of aids (e.g. movement splints, orthoses or crutches).
After joint stiffening interventions, a six-week plaster immobilization is usually necessary, after stiffening operations in the area of the Spine often a corset has to be worn for long periods of time (8-12 weeks).
Course and prognosis
The onset and course of ankylosing spondylitis are insidious, with the greatest loss of function and damage likely occurring in the first 10 years of the disease. The main complaints of patients with regard to quality of life are stiffness, pain, fatigue and poor sleep.
Factors that make the course of the disease more likely are:
- involvement of the hip joint and knee joint
- an increased sedimentation rate (> 30mm in the 1st hour)
- low effectiveness of nonsteroidal anti-inflammatory drugs (NSAIDs)
- a limitation of the mobility of the lumbar spine
- an inflammation of the little finger and toe joints
- Oligoarthritis (inflammation of many joints at the same time)
- an onset of the disease before the age of 16.
Ankylosing spondylitis afflicts patients at a relatively young age, which means that the disease burden, which is often considerable, lasts for a long time. The therapeutic options for ankylosing spondylitis have so far been quite limited, but a significant improvement is expected from the relatively new TNF-alpha inhibitors.